

Learn what fungal infections are, why they develop, and how timely treatment can protect your skin and confidence.
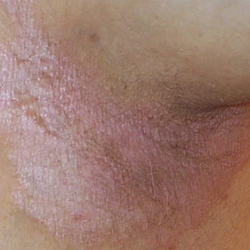
Fungal skin infections are caused by microscopic fungi that thrive in warm, moist environments such as skin folds, sweaty areas, and humid climates. They often appear as itchy, red, scaly patches and may spread if left untreated. Although common and usually manageable, ignoring them can lead to persistent discomfort and recurrence. Understanding the early signs and seeking the right care can help you regain healthy, irritation-free skin quickly and safely.
Patients Treated
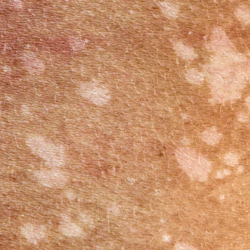
Fungal skin infections occur when naturally present fungi grow excessively on the skin and disrupt its normal balance. While fungi exist harmlessly on our body and in the environment, certain conditions like sweat, humidity, tight clothing, or poor ventilation allow them to multiply rapidly and cause infection. These infections can range from mild irritation to persistent and spreading rashes, commonly appearing as itching, redness, flaky patches, burning sensation, or discoloration. Because fungi thrive in warm and moist areas, they frequently affect the feet, groin, scalp, underarms, and skin folds. They can also spread easily through direct contact, shared clothing, towels, footwear, or contaminated surfaces.





Athlete’s Foot (Tinea Pedis) – Usually develops between the toes causing itching, peeling, and burning sensation.
Ringworm (Tinea Corporis) – Appears as circular, ring-shaped patches with clear centers and red borders.
Jock Itch (Tinea Cruris) – Affects the groin area leading to redness, irritation, and persistent itching.
Fungal Nail Infection (Onychomycosis) – Causes thick, brittle, discolored nails that may crumble over time.
Scalp Ringworm (Tinea Capitis) – Leads to scaly patches on the scalp and patchy hair loss.
Yeast Infection (Candidiasis) – Occurs in moist folds like underarms, under breasts, or groin with redness and soreness.
Tinea Versicolor (Pityriasis Versicolor) – Produces lighter or darker patches than the surrounding skin, especially on chest and back.
Although common, fungal infections should never be ignored — early identification and proper treatment help prevent spreading, recurrence, and long-term skin damage.
Fungal infections develop when the natural balance of microorganisms on the skin is disturbed, allowing fungi to grow uncontrollably. While fungi normally exist harmlessly on our body, certain internal and external factors create the perfect environment for them to multiply. Understanding these triggers helps in both prevention and long-term management of recurring infections.
A weakened immune system makes it harder for the body to fight fungal growth, increasing susceptibility.
Damp skin, excessive sweating, tight clothing, and humid weather create an ideal breeding ground for fungi.
Shared towels, socks, footwear, gym equipment, or public washrooms can transfer fungal spores to your skin.
Infrequent cleaning or skin areas that remain covered and unventilated allow fungi to flourish.
Treating fungal skin infections requires more than just temporary relief — it needs an accurate diagnosis and a targeted treatment plan. A dermatologist evaluates the infection type, severity, recurrence pattern, and lifestyle factors before recommending the most effective therapy. Early treatment prevents spreading and reduces chances of recurrence.
Consultation: Visit a dermatologist for a detailed skin examination. The doctor identifies the infection type, affected areas, and visible symptoms.
Evaluation: Your medical history, daily habits, hygiene practices, and any underlying health conditions are reviewed to determine triggers and recurrence causes.
Customized Treatment: A personalised treatment plan is prescribed — which may include topical medications, oral medicines, and preventive care tailored to your skin and infection severity.
Timely medical treatment not only clears the infection but also helps prevent repeated flare-ups and protects surrounding skin areas.

Fungal infections may start as mild itching or discoloration, but they rarely resolve on their own. Delayed treatment can allow the infection to spread deeper into the skin, nails, or scalp and make it harder to cure. Consulting a dermatologist at the right time helps prevent recurrence, transmission, and long-term damage.
The rash continues even after using over-the-counter antifungal creams.
The infection spreads to nearby skin, nails, or scalp areas.
You notice pain, swelling, cracks, bleeding, or oozing fluid.
The itching becomes intense and interferes with daily activities or sleep.
The infection keeps returning again and again after temporary relief.
You have diabetes, low immunity, or other medical conditions increasing infection risk.
Early diagnosis ensures faster healing, reduces transmission to others, and prevents stubborn, recurring fungal infections.
Speak with our dermatology specialists to understand the exact diagnosis and get a personalized treatment plan designed specifically for your fungal skin infection and skin type.
Book Consultation
Fungal skin infections are common, but they don’t have to become a recurring part of your life. With timely diagnosis and the right treatment plan, healthy and comfortable skin is absolutely achievable. Instead of letting the infection spread or return again and again, take the first step toward lasting relief — schedule your consultation and restore your skin’s balance.
- Reviewed by

Dr. Supratim Karmakar Consultant Dermatologist